Students showcase prototypes at Design Day
The 2017 Biomedical Engineering Design Day drew hundreds of students, faculty, clinicians, and mentors to the Johns Hopkins Medical Campus. Eight master’s student teams and 14 undergraduate student teams represented the Center for Bioengineering Innovation and Design with projects spanning a range of clinical topics.
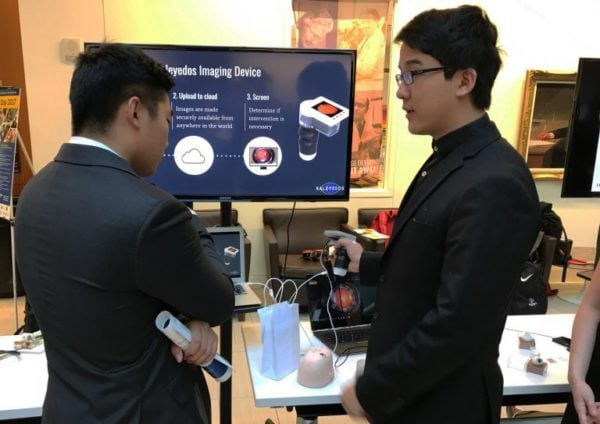
The event opened with a keynote address from Howard Levin and Mark Gelfand, co-founders of Coridea, a medical device incubator. Each team of students presented their projects, followed by a poster session and reception. Attendees were given the opportunity to interact with students, ask questions, and get a first-hand look at prototypes.
After hearing details from each team, attendees cast their vote for the People’s Choice Awards.
First place: PCN Medical
Making penicillin allergy testing available for large-scale implementation
CBID Master’s Team: Tessa Bronez, Katherine Czerniejewski, Katie Kan, Arman Mosenia, Doran Walsten, and Rachel Yung
Broad-spectrum antibiotics are known to result in more resistant organisms connected to antibiotic resistance. They are commonly prescribed to the 30 million Americans reporting a penicillin allergy, even though 90% of this population may not actually be allergic. PCN Medical addresses this challenge with a software application that determines the likeliness of a positive penicillin allergy for a patient, given his or her clinical history and an automated precision injection technology. This supplies healthcare professionals with the information needed to move forward with a testing and treatment protocol.
Second place: NeMo
Empowering mothers to identify neonatal illness
CBID Master’s Team: Rachel An, Andrew Jann, Matthew Lerner, Polly Ma, Mohit Singhala
Approximately 2.7 million newborns die each year, with 75% of these deaths occurring during the first week of life. In many developing countries, community healthcare workers make in-home visits to assess a neonate during this high-risk period, looking for symptoms outlined in World Health Organization guidelines. With limited health care workers and infrequent visits, many sick infants may be identified too late for treatment. NeMo (neonatal monitoring) gives mothers the tools to identify neonatal illness themselves. A smartphone application guides the mother through assessment, while a disposable sensor measures respiratory rate and temperature.
Third place: Kubanda
A carbon dioxide-based breast cancer treatment device for use in low-resource settings
CBID Undergraduate Team: Bailey Surtees, Clarisse Hu, Serena Thomas, Sean Young, Tara Blair, Evelyn McChesney, Grace Kuroki, Pascal Acree, Shivam Rastogi
Diagnosing breast cancer is a long-standing problem, especially in low and middle-income countries where access to health care is limited. In rural areas, the high costs and inaccessibility of treatment can often cause women to delay screening. While the five-year survival rate for breast cancer in the United States is nearing 90%, the survival rate is between 40% and 50% in rural South Africa. Kubanda is designing and optimizing a low-cost novel cryoablation device to freeze breast cancer cells. The device aims to make breast cancer treatment available to women living in low-resource, rural settings.
– Sarah Tarney
