Drug crystals to prevent medical device fibrosis
Implanted medical devices can save lives, but can also put patients at the risk of fibrosis, a condition in which the immune system attacks the device and produces scar tissue around it, interfering with the device’s functionality.
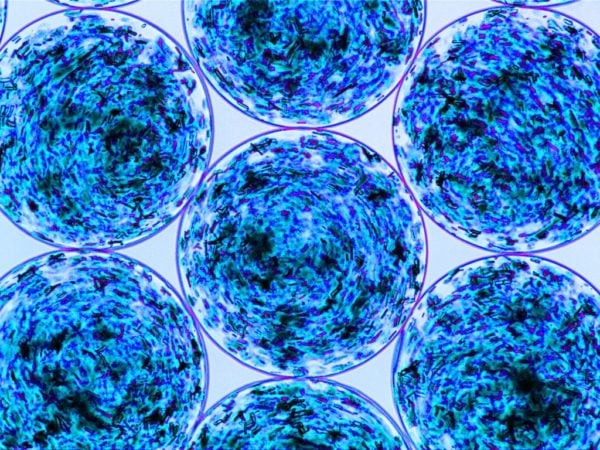
Working with researchers at Massachusetts Institute of Technology, Joshua Doloff, an assistant professor of biomedical engineering at Johns Hopkins University and former MIT postdoc, has devised a new way to prevent fibrosis: loading implantable devices with a crystallized immunosuppressant drug, which is slowly released into the patient’s system, inhibiting the immune response in the area surrounding the device.
“The drug crystal formulations allowed for tightly controlled, local, and long-term release to the point where we don’t really see any drug in global serum or plasma levels beyond the first few days, eliminating the possibility of side effects in other tissues of the body,” said Doloff.
In a paper published in a recent issue of Nature Materials, the researchers showed that this coating could dramatically improve the performance of encapsulated islet cells, which they are developing as a possible treatment for patients with type 1 diabetes. Encapsulated islet cells are special primary tissue or stem cell-derived grafts that are enclosed in a protective capsule before being implanted in the body with the purpose of eventually producing insulin.
Doloff’s team believes that such strategies also could be applied to a variety of other implantable medical devices, including pacemakers, stents, or sensors, the last of which was demonstrated in practice in the study.
“We showed that the drugs released very slowly and in a controlled fashion,” says Shady Farah, an MIT and Boston Children’s Hospital postdoc and co-first author of the paper. “We took those crystals and put them in different types of devices and showed that with the help of those crystals, we can allow the medical device to be protected for a long time, allowing the device to keep functioning.” Farah will soon serve as an assistant professor of the Wolfson Faculty of Chemical Engineering and the Russell Berrie Nanotechnology Institute at Technion-Israel Institute of Technology.
Doloff and Farah are working on ways to encapsulate islet cells and transplant them into diabetic patients, in hopes that such cells could replace the patients’ nonfunctioning pancreatic cells and eliminate the need for daily insulin injections.
Daniel Anderson, an associate professor in MIT’s Department of Chemical Engineering, and a member of MIT’s Koch Institute for Integrative Cancer Research and Institute for Medical Engineering and Science (IMES), is the senior author of the paper.
