Students in the Johns Hopkins Department of Biomedical Engineering’s Design Team program have developed a new tool for improving the assessment of damaged nerves during surgery.
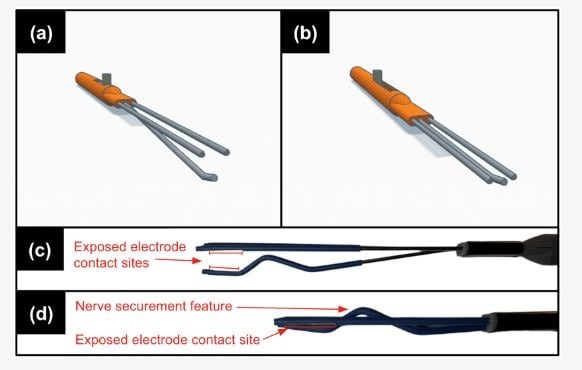
The innovation is a set of electrodes designed to work without having to move or lift the nerve during evaluation, promising to reduce patient injury and inaccurate readings.
Their work appears in the Web of Science indexed journal Healthcare.
“The tangible effects of our innovation contribute to a streamlined neurosurgical workflow, mitigate the risk of patient injury, and better inform treatment decision-making. Overall, this will help decrease patient recovery time and maximize peripheral nerve regeneration and recovery,” said Nathaniel Riemann ENGR ’23, the paper’s lead author.
A peripheral nerve injury occurs when nerves are crushed or stretched during physical trauma. To assess this injury, surgeons insert electrodes into the body, noting whether the injured nerves respond to a small electrical pulse. If they do, this indicates that the nerve is still functional and can regenerate on its own. The absence of a signal tells the surgeon that the nerve will not be able to regenerate, and that surgery is required.