Some heart disease patients face a higher risk of sudden cardiac death, which can happen when an arrhythmia—an irregular heartbeat—disrupts the normal electrical activity in the heart and causes the organ to stop pumping. However, arrhythmias linked to sudden cardiac death are very rare, making it difficult to study how they occur—and how they might be prevented.
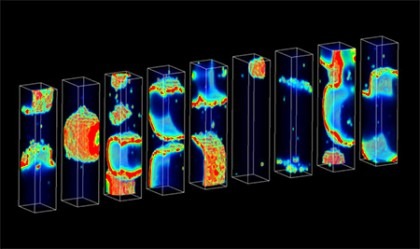
To make it much easier to discover what triggers this deadly disorder, a team led by Johns Hopkins researchers constructed a powerful new computer model that replicates the biological activity within the heart that precedes sudden cardiac death.
In a study published recently inPLOS Computational Biology, the team reported that the digital model has yielded important clues that could provide treatment targets for drugmakers.
“For the first time, we have come up with a method for relating how distressed molecular mechanisms in heart disease determine the probability of arrhythmias in cardiac tissue,” said Raimond L. Winslow, a professor in the Department of Biomedical Engineering at Johns Hopkins and senior author of the study.
“The importance of this is that we can now quantify precisely how these dysfunctions drive and influence the likelihood of arrhythmias. That is to say, we now have a way of identifying the most important controlling molecular factors associated with these arrhythmias.”
With this knowledge in hand, Winslow said, researchers will be better able to develop a treatment to keep some deadly heart rhythms from forming.
The lead author of the study was Mark A. Walker, who worked on the problem while earning his doctoral degree under Winslow’s supervision. Walker said he and his colleagues used computer models to determine what activity was linked to arrhythmia at three biological levels: in the heart tissue as a whole, within individual heart cells, and within the molecules that make up the cells, including small proteins called ion channels that control the movement of calcium in the heart.