Returning to sports too soon after a concussion or other traumatic brain injury (TBI) can increase the risk of an even more serious injury and long-term brain damage. Johns Hopkins biomedical engineering students have developed a new virtual reality (VR) game that provides athletes with objective data to guide return-to-play (RTP) decisions after a concussion, offering a more reliable alternative to current protocols that rely heavily on subjective inputs like self-reported questionnaires from the athlete.
“Our technology provides clinicians and athletic trainers with valuable insights into TBI recovery currently not captured by conventional tools,” said Shalika Subramanian, a fourth-year biomedical engineering student and team lead for the project. “The system transforms the usual clinical tests into an engaging game environment that generates objective, quantifiable and personalized recovery metrics.”
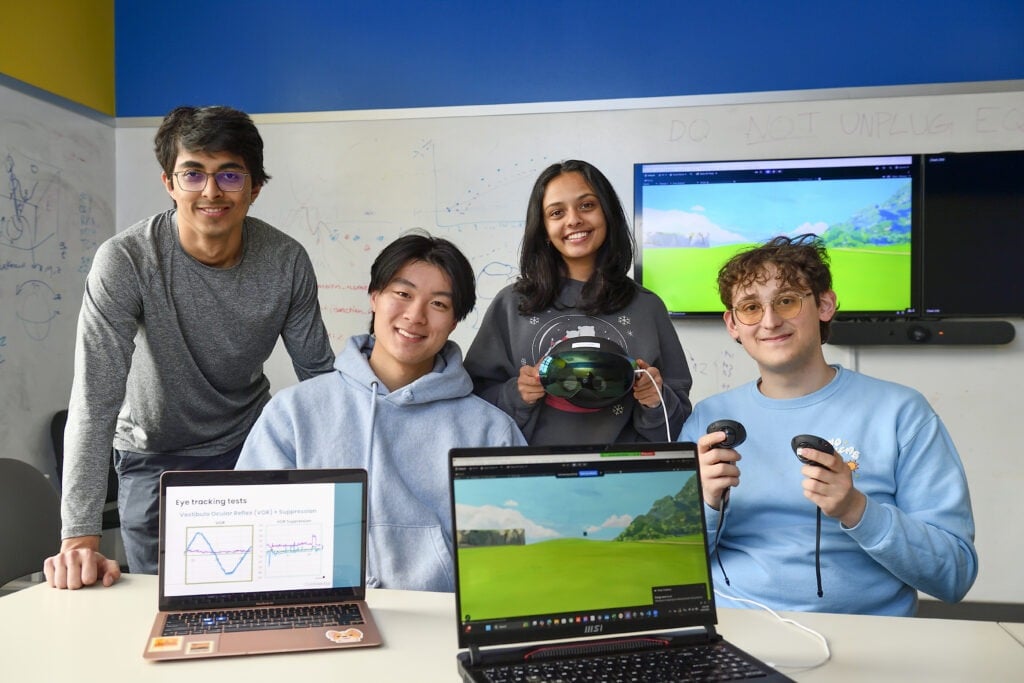
Subramanian and teammates Betania Arce, Arya Kazemnia, Issac Kim, Aditya Kondepudi, Divyansh (Dev) Lalwani, Pratibha Pradeep, and Edmund Tsou will present their work on Tuesday, April 29, at the Johns Hopkins Engineering Design Day—the annual year-end event showcasing students’ solutions to real-world problems.
The device works like this: An athlete wears the VR headset and runs through a series of mini-games that test eye-tracking, balance, motor skills, and cognition — all brain functions typically impaired after a TBI. For example, one such game includes tracking a randomly generated ball that moves across the landscape that the athlete must follow with their eyes. If they accurately track it, the ball will disappear for a second before reappearing in a new spot and repeating until the test is complete.
Comprehensive recovery data captured by the headset is securely uploaded onto a cloud-based platform, giving clinicians and trainers access to objective measurements that enable more data-driven RTP decisions rather than relying solely on patients’ reported symptoms.