Student engineers in the Johns Hopkins Biomedical Engineering Design Team program have invented a new system to detect hemorrhagic shock early in traumatically injured children, who can lose a significant amount of blood before symptoms appear. Their innovation, called ShockSense, could help clinicians act faster in cases where a child might lose their entire circulating blood volume in under five minutes—risking severe complications or death.
“Children compensate for blood loss better than adults and mask the early signs of shock. As a result, delayed recognition can result in higher mortality and increased risk of complications for pediatric patients,” said team leader Ella Holtermann, a third-year biomedical engineering student.
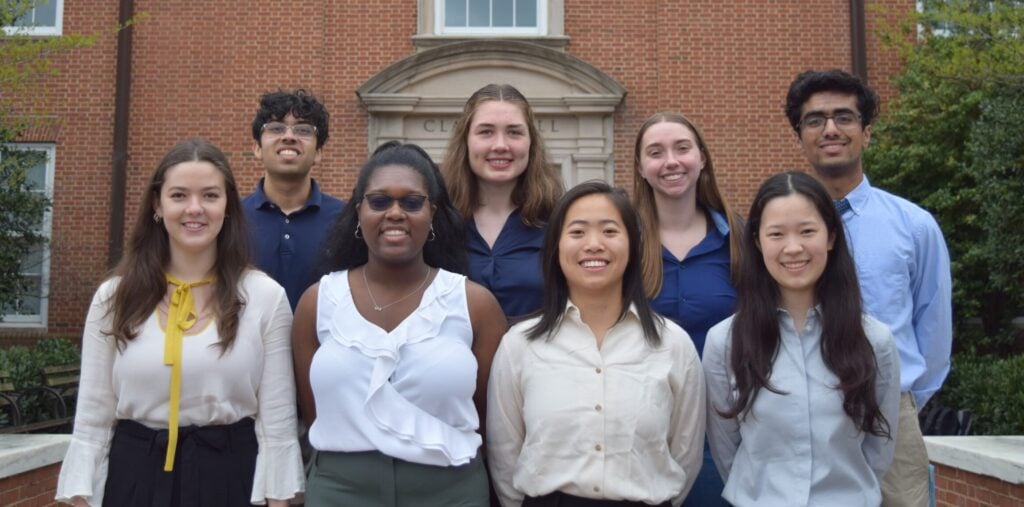
She and team members Loren Ayers, Isabella Godfrey, Vivien Jiang, Elizabeth Zuerblis, Ashrith Kollu, Aditya Sinha, and Apple Wu will present their innovation on April 29 at the Whiting School of Engineering’s Design Day, an annual event showcasing students’ solutions to real-world problems.
ShockSense is a device that analyzes real-time vitals to identify signs of shock and suggest treatment procedures—streamlining care while clinicians focus on delivering life-saving interventions.
Currently, determining whether a child needs a blood transfusion involves evaluating a patient’s vital signs against age-based norms. This method can be challenging in high-stakes trauma situations, requiring memorization of the normal range of vital signs and consideration of the variability in vital signs across children of different ages. For example, the expected heart rate and blood pressure of a six-year-old can differ significantly from that of a twelve-year-old.