Testing the algorithm
To build and test their approach’s predictive abilities, the team studied three sources of waveform data that are continuously collected from ICU patients: arterial blood pressure (ABP), electrocardiogram (ECG), and photoplethysmography (the signal used for pulse oximetry recordings). They started with a dataset of patients who had simultaneous measurements taken of these variables and invasive ICP measurements obtained via catheters in the brain. Next, they used ABP, ECG, and PPG waveforms to train six different deep-learning algorithms to see if they could generate ICP waveforms that were accurate when compared to the “ground truth” ICP measured using invasive methods.
It worked. The ICP values estimated using the new algorithm closely matched those measured using invasive methods. What’s more, the Hopkins algorithm was as accurate as, or even more accurate than, other non-invasive methods for evaluating ICP.
These results are quite significant, according to Stevens, who points out that a method that allows for continuous, real-time non-invasive ICP monitoring could spare patients from a risky surgery and let physicians know when they must intervene to decrease ICP.
“If further studies confirm that this is reliable and accurate, maybe we can do away with the invasive ICP monitoring altogether,” said Stevens. “What’s also exciting is that this would mean ICP could be monitored in various care settings, and not just in an intensive care unit.”
The team plans to validate these findings using a much larger dataset before moving on to enrolling a cohort of patients for a prospective trial. Many of the students, including Nair, have continued to work on the project even after moving on to other institutions or industry positions.
“It’s been remarkable to see how something that started as a class project ended up here. It’s a testament to the motivation and engagement of our students that we’ve arrived at a result that is, in many ways, a great success,” said Stevens.
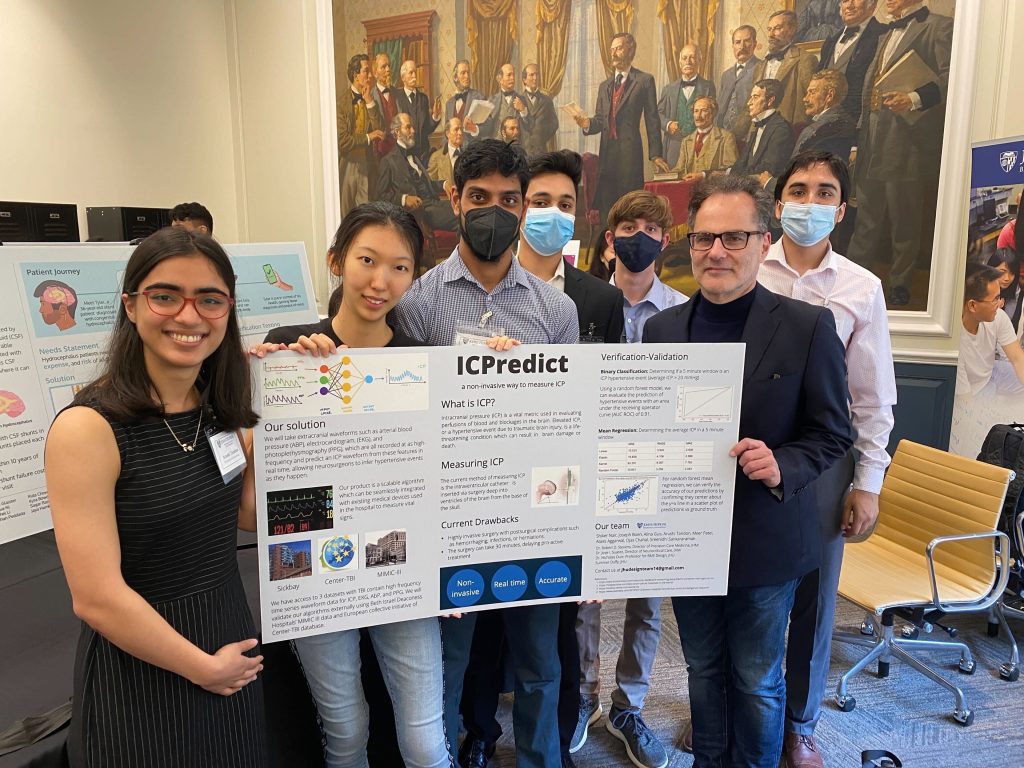
Additional co-authors include recent Hopkins alums Alina Guo ’23, Arushi Tandon ’23, and Joseph Boen ’22; master’s student Meer Patel; biomedical engineering seniors Atas Aggarwal, Ojas Chahal, and Sreenidhi Sankararaman; Tej D. Azad, a resident physician in the Johns Hopkins Department of Neurosurgery; and Romain Pirracchio, a professor of anesthesia at The University of California, San Francisco (UCSF).