For the more than 15 million epilepsy patients around the world whose disease is not controlled by medication, the only remaining option is removal of the parts of the brain where seizures originate. Even then, surgery is only 50% effective because accurately pinpointing the brain regions responsible is challenging.
Developed by Johns Hopkins University biomedical engineers, a new method of highlighting the most epileptic parts of the brain could enable not only more accurate diagnosis of the seizure disorder, but also help guide more precise surgical treatment. The team’s study was published recently in Nature Neuroscience and was featured on the cover.
“For these patients, the only available treatment is to surgically remove the brain area responsible for seizures,” said study first author Adam Li, a doctoral student in the laboratory of Sridevi Sarma, associate professor of biomedical engineering. “However, surgery is not as effective as it should be because there is no biomarker that can pinpoint the epileptic brain regions. Our goal was to solve that problem.”
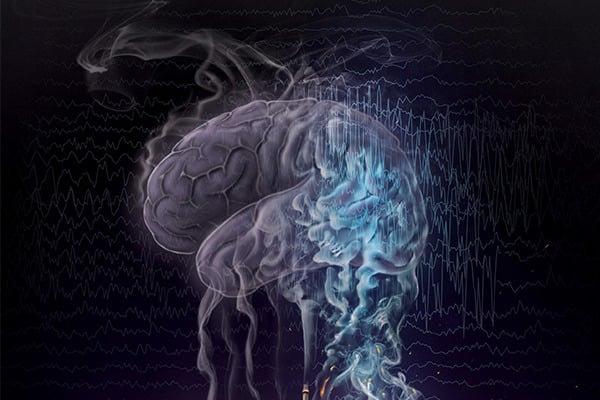
In the study, the team describes how they modeled the dynamics of brain waves to develop a quantitative test that calculates the likelihood that any single brain region would contribute to a seizure. The mathematical model was based on biological experiments that showed changes in brain region connections that render the brain unstable, and thus, prone to seizures. This instability is known as neural fragility. The team then applied this mathematical model to data from electroencephalograms (EEG), computing neural fragility for every EEG electrode.